Superior canal dehiscence (SCD) refers to the lack of bone covering the superior balance canal, so that the inner ear soft tissue lining is in contact with the brain lining. Normally dense bone covers these balance canals. Where sound normally goes into the bony inner ear (through the oval window) and exits (through the round window). This creates a “third window effect with excessive sound waves amplifying or cancelling each other which sometimes creates symptoms.
Causes
Two theories are proposed:
Congenital – where there is a defect in bone formation between the inner ear and brain at birth. The bone in the first few years does not close off.
Acquired – Higher intracranial pressure may wear the bone between the inner ear and brain. Trauma may also unmask the symptoms.
Symptoms
A lot of patients have SCD but no symptoms. When symptoms are associated with the anatomical defect then the condition is called Superior Canal Dehiscence Syndrome (SCDS). If a patient has concurrent migraine, otosclerosis or bilateral SCDS, then postop improvement is not as predictable.
Classic symptoms include:
- Autophony (>50% patients) – hearing your own voice in the ear when speaking or internal bodily noises loudly such as chewing, eyeballs moving or footsteps.
- Sound or pressure induced dizziness/ vertigo (>50%)
- Fullness in the ear (>50%) or Brain “fog” from chronic imbalance.
- Pulsating ringing in ear (pulsatile tinnitus) (20-50%)
- Hearing loss (20-50%) or hyper-sensitive hearing (20-40%)
Signs
- Imbalance or eye movement with pressure on the ear canal
- Sometimes patients have a conductive hearing loss on tuning forks and occasionally the patient can hear the tuning fork when placed on the knee or ankle.
Diagnosis
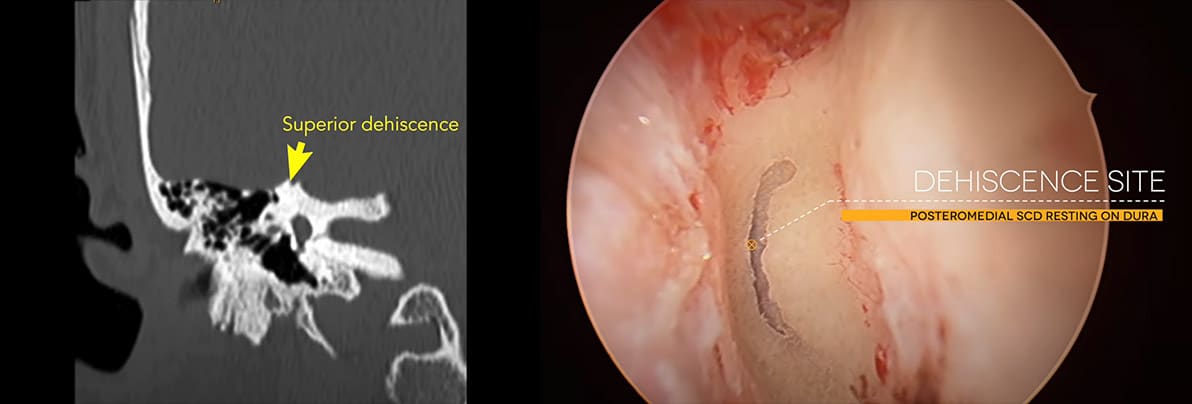
CT Scan – high resolution thin slice (<0.625mm) is the essential investigation to diagnose the condition. Posch and Stenver’s views are especially useful.
MRI may be requested to exclude other conditions, to check postop outcomes and in revision cases.
Hearing Tests – classically a conductive hearing loss is found in low frequencies with normal stapedial reflexes. A negative bone conduction is often found.
Balance tests – Reduced cVEMPs and Elevated oVEMPS. Other balance tests such as calorics and VORs are useful to help predict postop outcomes, especially if there are preoperative abnormalities.
ECoG – Elevated SP to AP ratio with no sensorineural hearing loss
Treatment
Most patients with SCDS do not seek surgical treatment, with large European and US centres seeing about half of symptomatic patients will be distressed enough to seek an operation. Most patients will just avoid loud sounds.
Surgery either recreates the bone over the canal (resurfacing) or blocks off (occludes) the canal so that not as much sound can be transmitted through the inner ear. Long term follow up in unit that resurface and occlude has shown more robust outcomes with occlusion.
Three broad surgical approaches have been published:
Round Window closure
Is a simple, through the ear canal, method to reduce the third window effect but NOT treat the actual SCD. The operation is day surgery with minimal pain. The long-term success rate to reduced symptoms is between 20-40% at 12 month follow up. Few patients have a permanent complete resolution. There is a small risk of conductive hearing loss with this method.
Transmastoid
Is a less invasive definitive technique to treat the SCD, when compared to the originally described middle fossa approach. It is used when the anatomy is favourable to reach the SCD from an approach behind the ear. It is my preferred approach if the anatomy is appropriate. The technique is a day surgery operation that requires a cut behind the ear and then drilling to get to the superior balance canal.(Link to my youtube video here) The canal is then typically occluded but can occasionally be resurfaced with this method. In units that perform both the middle fossa and transmastoid approach, the hearing and symptoms resolution outcomes are not statistically different. There is around an 80% chance of symptoms improvement or resolution. With published improvement in quality of life and objective measures of SCDS.
Middle Fossa Approach
Is the original described operation which requires a craniotomy (opening the skull above the ear), and elevating the brain to observe the actually SCD from above and then occlude or resurface. This is the method I use, when the anatomy is not suitable for the transmastoid approach.
The success rate is above 80% however this method does have a higher risk of brain surgery complications such as CSF leak, meningitis and bruising to the brain, when compared to the transmastoid approach.
Expected Common Complications after Transmastoid or Middle Fossa surgery
Hearing loss – 25% of patients have a high frequency hearing loss which is often permanent
Benign positional vertigo occurs in 25% of patients and usually settles in a few months.
Imbalance occurs in 30-40% of patients transiently and significant percentage can have more longstanding dizziness especially if they have migraine, otosclerosis or Bilateral SCD.
Postoperative period
Steroids (for a couple of weeks) and balance therapy for a few months is often recommended after surgery.
The transmastoid approach is usually day surgery or an overnight stay in hospital. Depending on work circumstances usually 2 weeks off work is required and driving is allowed with in 2-3 days if there is no imbalance.
The middle fossa approach usually requires 1 night in ICU (intensive care) and then a few days in hospital. Depending on work circumstances 2-4 weeks off is required. Driving is decided depending on healing and balance recovery.
OTHER DISEASE PROCESSES
Got a question you would like to ask Dr Nirmal Patel?
